Medical Billing for Behavioral Health
September 22, 2025
Provider Credentialing: The Step-by-Step Process
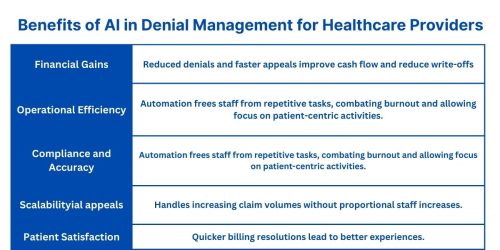
October 7, 2025Artificial intelligence (AI)—a game-changer that’s revolutionizing denial management in medical billing. AI leverages machine learning, natural language processing (NLP), and predictive analytics to preempt issues, automate workflows, and provide actionable insights. In the fast-paced world of healthcare revenue cycle management (RCM), denial management stands as a critical yet challenging process. For medical billing companies like Skyshine Health Solutions, effectively handling claim denials can mean the difference between financial stability and significant revenue loss. As of 2025, claim denials average between 5% to 10% of all submissions, according to industry reports, leading to billions in lost revenue annually across the U.S. healthcare system. Traditional methods, reliant on manual reviews and reactive appeals, are increasingly inadequate in the face of rising denial volumes, complex payer policies, and stringent regulations.
AI not only reduces denial rates but also accelerates reimbursements, enhances compliance, and frees up billing teams for more strategic tasks. In this comprehensive guide, we’ll explore how AI is transforming denial management, backed by the latest 2025 trends, real-world examples, and practical implementation strategies. Whether you’re a healthcare provider, billing specialist, or RCM executive, understanding these advancements can help optimize your operations and boost your bottom line.
The Challenges of Traditional Denial Management in Medical Billing
Before diving into AI’s transformative role, it’s essential to understand the pain points of traditional denial management. In medical billing, denials occur when payers reject claims due to errors in coding, insufficient documentation, lack of medical necessity, or non-compliance with ever-evolving policies. According to recent analyses, up to 82% of denials are avoidable, yet they persist due to systemic inefficiencies.
- Manual processes dominate traditional approaches:
billing teams review denied claims individually, categorize them using spreadsheets, and craft appeals based on historical knowledge. This is time-intensive—appeals can take weeks or months—and prone to human error. Common challenges include:
- Lack of Real-Time Visibility:
Without advanced tools, teams struggle to track denial trends in real time, leading to recurring issues.
- Complex Payer Policies:
Payers frequently update rules, making it hard to stay compliant without constant vigilance.
- High Administrative Burden:
Staff spend hours on data entry, error correction, and follow-ups, contributing to burnout and reduced productivity.
- Revenue Leakage:
Delayed or abandoned appeals result in write-offs, with some practices losing up to 20% of potential revenue.
Scalability Issues: As claim volumes grow—driven by telehealth expansions and chronic care management—manual systems can’t keep pace.
These hurdles not only strain resources but also impact patient care, as delayed payments can limit service availability. In 2025, with healthcare costs rising and regulations tightening (e.g., CMS updates to HCC models), the need for innovation is more urgent than ever. AI addresses these by shifting from reactive to proactive strategies, automating routine tasks, and providing data-driven foresight.
Key Ways AI is Revolutionizing Denial Management
AI’s integration into denial management is multifaceted, drawing on technologies like machine learning (ML), NLP, and robotic process automation (RPA). Here’s how it’s making waves in 2025, based on emerging trends and expert insights.
1. Predictive Analytics for Denial Prevention
One of AI’s most powerful contributions is its ability to predict and prevent denials before claims are submitted. By analyzing vast datasets of historical claims, AI identifies patterns in denials—such as frequent coding errors or payer-specific rejections—and flags high-risk claims in real time.
For instance, ML algorithms scan for discrepancies in patient data, billing codes, and documentation, suggesting corrections upfront. This “claim scrubbing” process uses NLP to extract insights from clinical notes, ensuring medical necessity is clearly demonstrated. Benefits include a potential 40% reduction in denial rates, faster first-pass approvals, and improved cash flow.
In 2025, predictive models are evolving with enhanced data integration, incorporating real-time payer updates via APIs. This allows AI to forecast denial risks based on current trends, such as shifts in telehealth billing guidelines, preventing issues that could otherwise lead to revenue delays.
2. Automated Error Detection and Claim Accuracy Enhancement
AI excels at boosting claim accuracy by automating data validation and error detection. Traditional manual checks are error-prone, but AI systems instantly verify details like patient eligibility, service codes (e.g., CPT, ICD-11), and prior authorizations.
Using NLP, AI processes unstructured data from electronic health records (EHRs) to assign accurate codes, reducing undercoding or overcoding—common denial culprits. For example, if a claim lacks supporting documentation for a procedure, AI can alert the team or even auto-generate the required notes based on historical successes.
This automation not only minimizes rework but also ensures compliance with HIPAA and CMS regulations. Providers report up to 97% time savings in coding tasks, allowing staff to handle more claims efficiently. In 2025, AI’s role here is amplified by blockchain integration for secure data sharing, further streamlining multi-payer interactions.
3. Streamlining the Appeals Process with Automation
Once a denial occurs, AI transforms the appeals workflow from a manual slog to an efficient, automated system. AI analyzes denial reasons, cross-references them with past successful appeals, and generates customized appeal letters complete with supporting evidence.
Tools prioritize appeals based on success likelihood and urgency, using ML to learn from payer behaviors. For high-volume denials, AI categorizes them (e.g., coding vs. authorization issues) and automates submissions, tracking progress in real time.
This reduces appeal turnaround from months to days, increasing reimbursement rates. A key benefit is reduced administrative burden—RCM teams can focus on complex cases while AI handles 80-90% of routine appeals. Looking to 2025, AI will incorporate voice-activated appeals and RPA for seamless EHR updates, making the process even more user-friendly.
4. AI-Driven Insights for Better Decision-Making
AI provides deep analytics that empower data-driven decisions in denial management. By processing large volumes of claims data, it uncovers root causes—such as recurring payer-specific trends or operational weaknesses—and delivers real-time alerts.
For example, dashboards highlight denial rates by code or provider, enabling proactive training or policy adjustments. This insight-driven approach prevents future denials, optimizing overall RCM.
In 2025, with 46% of organizations already using AI for RCM and 49% planning adoption, these insights will integrate with predictive tools for holistic revenue forecasting. Benefits include refined billing practices and up to $1.14 million in annual recovered revenue from missed codes.
5. Seamless Integration with RCM Systems
AI’s true power lies in its ability to integrate with existing RCM platforms, creating end-to-end visibility. From claim submission to resolution, AI automates workflows, improves inter-departmental coordination, and scales with practice growth.
Cloud-based AI solutions connect with EHRs like EPIC or Athena, ensuring data flows securely. This integration reduces silos, accelerates resolutions, and supports remote teams—a boon in post-pandemic healthcare.
Real-World Examples and Case Studies
Real-world applications underscore AI’s impact. In one case, a large hospital network implemented AI for denial prediction, reducing denials by 30% within six months by flagging coding errors pre-submission.
GaleAI, an AI tool, helped a provider recover $1.14M annually by identifying missed codes in historical data. Another example from Banner Health involves AI in appeals, streamlining processes and improving success rates at 2025 conferences.
BDO’s use cases show AI automating prior authorizations, addressing a 20% denial surge without added staff. These examples illustrate AI’s versatility across practice sizes.
Implementation Guide: Integrating AI into Your Denial Management Workflow
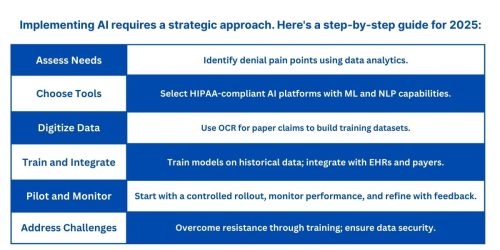
Challenges include integration costs and staff adaptation, but benefits outweigh them with proper planning.
Future Trends in AI for Denial Management in 2025 and Beyond
In 2025, AI will evolve with blockchain for secure transactions, advanced NLP for ICD-11 transitions, and predictive models incorporating social determinants of health. Expect full automation of appeals, AI-driven compliance checks, and integration with telehealth billing. As adoption grows, denial rates could drop below 5%, transforming RCM into a proactive powerhouse.
Conclusion: Embrace AI for Smarter Denial Management
AI is not just enhancing denial management—it’s redefining it, turning a revenue drain into a strategic asset. For medical billing companies like Skyshine Health Solutions, leveraging AI means fewer denials, faster payments, and sustainable growth. If you’re ready to optimize your RCM, contact us today for tailored AI solutions that fit your practice. Let’s turn denials into approvals—together.

For related blog, check The Role of AI in Medical Billing and Coding Compliance
Visit Skyshine Health Solutions for more.