Key Differences Between Credentialing And Enrollment
October 13, 2025In the fast-evolving healthcare landscape of 2025, where regulatory changes and digital advancements are reshaping revenue cycle management (RCM), provider credentialing remains a linchpin for financial success. As a leading medical billing company, Skyshine Health Solutions has seen firsthand how credentialing mistakes can cripple practices, leading to delayed approvals, denied claims, and substantial revenue losses. With CMS introducing consolidated CMS-855 forms and stricter requirements for new provider types like Marriage and Family Therapists (MFTs) and Mental Health Counselors (MHCs), avoiding mistakes is critical. Payers like Aetna and UnitedHealthcare are also tightening verification protocols, making precision non-negotiable.
Credentialing verifies a provider’s qualifications, ensuring they can bill insurers and deliver compliant care. Yet, errors in credentialing process can cost practices $100,000-$250,000 per provider annually due to unbilled services and denials. This comprehensive 3000-word guide explores the top 5 common credentialing mistakes, their impact on your billing revenue, and actionable strategies to avoid them. Tailored for healthcare providers, practice managers, and billing professionals, this blog leverages 2025 insights to optimize RCM. At Skyshine, we’ve helped practices recover millions by streamlining credentialing—let’s dive in to safeguard your bottom line.
Why Credentialing Matters for Medical Billing in 2025
Provider credentialing is the process of verifying a healthcare professional’s qualifications—education, licenses, certifications, and professional history—through Primary Source Verification (PSV) and platforms like CAQH ProView. It ensures compliance with hospital, payer, and regulatory standards, enabling providers to enroll with insurers and bill for services. In 2025, credentialing is more complex due to:
-
- CMS Updates: Consolidated CMS-855 forms streamline submissions but require precise data for SNFs and new provider types like MFTs.
- Payer Scrutiny: Private insurers demand quarterly CAQH updates and stricter PSV.
- Telehealth Growth: Expanded telehealth regulations require additional credentialing for virtual care providers.
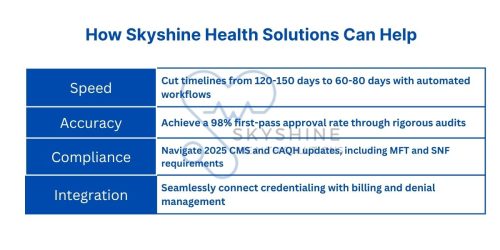
Errors in credentialing disrupt billing, leading to claim denials, audits, and patient churn. A 2024 study found that 65% of practices face delays, costing $7,000-$10,000 per week per provider. Skyshine’s outsourcing services achieve a 98% first-pass approval rate, cutting timelines by 40% and ensuring compliance. By avoiding the following mistakes, you can protect revenue and focus on patient care.
Mistake 1: Incomplete Applications and Missing Documentation
Description: Submitting incomplete applications or missing critical documents—like state licenses, DEA registrations, board certifications, or malpractice insurance—is the most common credentialing error. This often results from rushed preparations, lack of checklists, or poor coordination.
How It Hurts Your Billing Revenue:
-
- Delayed Approvals: Incomplete submissions reset the 90-120 day credentialing timeline, extending it to 150+ days. Providers can’t bill insurers during this period, leading to $100,000-$250,000 in lost revenue per provider.
- Increased Denials: Payers reject claims from uncredentialed providers, with denial rates rising to 20-30% for practices serving Medicare patients.
- Administrative Costs: Resubmissions require additional staff time, costing $5,000-$10,000 per provider in labor.
- Audit Risks: In 2025, CMS’s focus on compliance means incomplete applications trigger audits, with fines up to $50,000 for non-compliance.
Actionable Strategies to Avoid It:
-
- Create a Checklist: Include NPI, CAQH profiles, licenses, certifications, CV, references, and 2025 CMS requirements for MFTs and MHCs.
- Use Digital Tools: Platforms like Symplr or Modio Health organize documents securely, reducing errors by 50%.
- Conduct Pre-Submission Audits: Skyshine’s free audits catch 99% of gaps before submission.
- Start Early: Begin 4-6 months before a provider’s start date to allow buffer time for corrections.
2025 Insight: Payers now use AI-driven reviews to flag incomplete applications instantly, increasing rejection rates. Skyshine’s proprietary software ensures 100% completeness, integrating with CAQH and PECOS for seamless submissions.
Deep Dive: Missing documents like malpractice insurance or peer references can delay hospital privileging, further impacting revenue. For example, a practice with 10 providers could lose $1 million annually if each faces a 2-month delay. By outsourcing to Skyshine, practices reduce this risk, with our team handling document collection and verification.
Mistake 2: Outdated Provider Information and CAQH Profiles
Description: Failing to update provider information—such as practice addresses, licenses, or CAQH ProView profiles—is a frequent oversight. CAQH, used by over 1,000 payers, requires quarterly updates, yet 70% of practices neglect this, leading to lapsed profiles.
How It Hurts Your Billing Revenue:
-
- Claim Denials: Outdated CAQH profiles cause immediate rejections, with 10-15% of claims denied until resolved, costing $50,000-$150,000 per provider.
- Re-Credentialing Delays: Lapsed profiles delay re-credentialing (every 2-3 years), halting billing for 1-3 months and reducing revenue by 20-25%.
- Compliance Penalties: In 2025, CMS and payers penalize outdated data, with fines up to $50,000 for non-compliance.
- Patient Churn: Delayed billing disrupts patient trust, with practices reporting 10-15% patient loss due to out-of-network status.
Actionable Strategies to Avoid It:
-
- Set Automated Reminders: Schedule CAQH updates 30 days before quarterly deadlines.
- Integrate with RCM Software: Skyshine’s platform syncs profiles in real-time, ensuring accuracy.
- Monitor 2025 Changes: Stay updated on CMS’s SNF data requirements and payer policies.
- Outsource Maintenance: Skyshine’s continuous monitoring prevents lapses, saving 10-15 hours per provider annually.
2025 Insight: Payers like Cigna now require real-time CAQH updates for telehealth providers, increasing scrutiny. Skyshine’s automated tracking ensures compliance, reducing denial risks by 95%.
Deep Dive: Outdated information exacerbates fraud risks, as payers use AI to detect discrepancies. A single lapsed profile can disrupt billing for multiple payers, compounding losses. For group practices, this can lead to $500,000+ in annual losses if not addressed promptly.
Mistake 3: Data Entry Errors and Transcription Mistakes
Description: Transcription errors, such as mismatched NPIs, TINs, or misspelled names, are common in manual submissions. These errors often stem from siloed systems or untrained staff, affecting 60% of credentialing applications.
How It Hurts Your Billing Revenue:
-
- Rejection Delays: Errors reset the review process, extending timelines by 4-6 weeks and delaying billing by $50,000-$100,000 per provider.
- Claim Denials: Mismatched data leads to 15-20% denial rates, with practices losing $30,000-$80,000 per provider annually.
- Audit Triggers: In 2025, CMS’s stricter PSV rules flag discrepancies, risking fines and network exclusions.
- Administrative Overhead: Correcting errors requires 20-30 hours of staff time, costing $2,000-$5,000 per incident.
Actionable Strategies to Avoid It:
-
- Use Automated Software: Tools like Modio Health minimize human error by 80%.
- Cross-Check Data: Verify NPIs and TINs via PSV before submission.
- Train Staff: Educate on 2025 CMS form consolidations and payer requirements.
- Outsource to Skyshine: Our audits catch 99% of errors pre-submission, ensuring accuracy.
2025 Insight: AI-driven payer reviews in 2025 flag even minor discrepancies, increasing rejection rates. Skyshine’s software aligns data across CAQH, PECOS, and payer systems, reducing errors to near zero.
Deep Dive: In group practices, a single error can affect multiple providers, leading to cascading denials. For example, a mismatched TIN for a 5-provider group could cost $500,000 if unresolved for 2 months. Skyshine’s rigorous checks prevent such scenarios.
Mistake 4: Missed Deadlines for Renewals and Re-Credentialing
Description: Failing to meet renewal deadlines for licenses, DEA registrations, or re-credentialing (every 2-3 years) is a common oversight due to poor time management or lack of reminders.
How It Hurts Your Billing Revenue:
-
- Billing Disruptions: Lapsed credentials halt billing, costing $10,000 per week per provider. A 2-month delay can lead to $80,000-$160,000 in losses.
- Re-Credentialing Delays: Missed deadlines extend re-credentialing by 1-3 months, reducing revenue by 15-25%.
- Compliance Fines: CMS and payers impose penalties up to $50,000 for lapsed credentials in 2025.
- Patient Impact: Billing disruptions force out-of-pocket payments, leading to 10% patient churn.
Actionable Strategies to Avoid It:
-
- Use Compliance Calendars: Track deadlines for licenses and re-credentialing.
- Set Automated Reminders: Schedule alerts 90 days in advance for renewals.
- Leverage Software: Skyshine’s platform automates deadline tracking, ensuring compliance.
- Outsource to Experts: Skyshine’s team manages renewals, preventing disruptions.
2025 Insight: Telehealth expansions in 2025 require timely renewals for virtual care credentials, with non-compliance risking exclusion from payer networks.
Deep Dive: Missed deadlines can trigger chain reactions, affecting payer enrollment and MIPS scores. Practices with 10 providers could lose $1 million annually if renewals lapse for multiple providers. Skyshine’s proactive monitoring eliminates this risk.
Mistake 5: Neglecting Primary Source Verification and Exclusion Checks
Description: Skipping PSV or failing to check OIG exclusion lists is a high-risk mistake. PSV confirms credentials directly with issuing sources, while OIG checks ensure providers aren’t sanctioned.
How It Hurts Your Billing Revenue:
-
- Claim Denials: Non-verified credentials lead to 100% denial rates, costing $100,000+ per provider.
- Retroactive Recoupments: Hiring excluded providers triggers clawbacks, with losses up to $300,000.
- Network Exclusion: In 2025, CMS’s fraud focus means exclusions bar federal program participation, slashing revenue by 40%.
- Legal Risks: Non-compliance risks lawsuits and fines, adding $50,000-$100,000 in costs.
Actionable Strategies to Avoid It:
-
- Mandate PSV: Verify all credentials with original sources, not secondary reports.
- Run Monthly OIG Checks: Use NPDB’s continuous query service for real-time updates.
- Train Staff: Educate on 2025 fraud prevention protocols.
- Outsource to Skyshine: Our verification process ensures 100% compliance, reducing risks.
2025 Insight: CMS’s 2025 anti-fraud initiatives increase scrutiny, with AI tools flagging unverified providers instantly. Skyshine’s rigorous PSV and OIG checks protect practices.
Deep Dive: Neglecting PSV can lead to patient safety concerns, damaging reputation and causing 15-20% patient loss. For large practices, this mistake can cost millions in combined revenue and legal fees.
The Financial Impact of Credentialing Mistakes
The cumulative effect of these mistakes is staggering. A single provider facing a 3-month delay due to incomplete applications, outdated profiles, or missed renewals could lose $120,000-$300,000. For a 10-provider practice, this escalates to $1.2-$3 million annually. Add in denials (10-30% of claims), audits ($50,000 fines), and patient churn (10-15%), and the impact is catastrophic. In 2025, with rising healthcare costs and value-based care tying reimbursements to compliance, these errors are costlier than ever.
Skyshine’s Impact: Our outsourcing services recover 85-90% of potential revenue by addressing these mistakes proactively. A recent client, a multi-specialty clinic in Texas, saved $500,000 by streamlining credentialing for five providers, reducing delays from 5 months to 65 days.
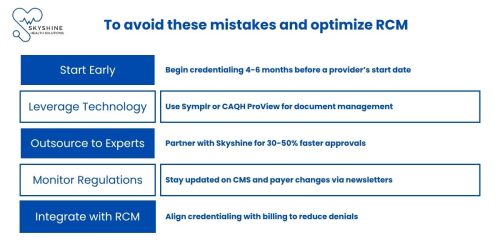
Best Practices for 2025 Credentialing Success
Conclusion: Protect Your Revenue with Flawless Credentialing
In 2025, avoiding credentialing mistakes is critical to maintaining billing revenue and compliance. Incomplete applications, outdated profiles, data errors, missed deadlines, and neglected verifications can cost practices millions. By implementing proactive strategies and partnering with Skyshine Health Solutions, you can streamline credentialing, reduce denials, and boost cash flow. Ready to safeguard your practice? Contact Skyshine today for a free credentialing audit and discover how we can optimize your RCM.
Click to view similar blog on Provider Credentialing: The Step-by-Step Process
Call to Action: Visit Skyshine Health Solutions to schedule your free consultation and eliminate credentialing errors in 2025.