Provider Credentialing: The Step-by-Step Process
October 7, 2025
Common Credentialing Mistakes and Impact on Billing Revenue
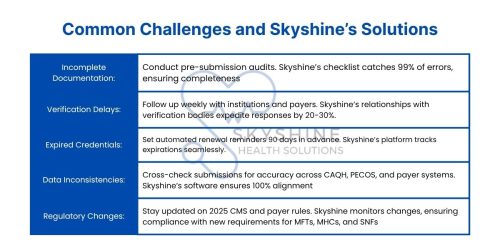
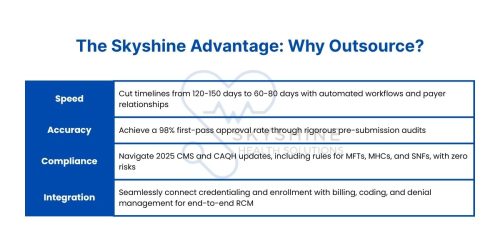
October 20, 2025In the fast-paced, regulation-heavy world of healthcare, administrative processes can make or break a practice’s financial health. Two critical components stand out: provider credentialing and payer enrollment. These processes are the backbone of effective revenue cycle management (RCM), ensuring providers can deliver care, bill insurers, and secure timely reimbursements. At Skyshine Health Solutions, a leading medical billing company, we’ve helped hundreds of practices streamline credentialing and enrollment, reducing timelines by up to 40% and boosting revenue with a 98% first-pass claim approval rate. But what exactly are these processes, how do they differ, and why are both indispensable in 2025?
This comprehensive guide dives deep into the nuances of the key differences between credentialing and enrollment, their roles in medical billing, and actionable strategies to optimize them. Tailored for solo practitioners, multi-specialty clinics, and hospital administrators, this blog leverages the latest 2025 updates from CMS, CAQH, and private payers to provide a clear roadmap. By mastering these processes, you can avoid costly delays, reduce claim denials, and enhance patient access. Let’s explore why credentialing and enrollment are the twin pillars of medical billing success and how Skyshine can transform your practice’s financial performance.
Understanding Provider Credentialing
Provider credentialing is the rigorous process of verifying a healthcare professional’s qualifications to ensure they meet the standards of hospitals, insurance payers, and regulatory bodies. It’s a safeguard for patient safety, legal compliance, and practice credibility, confirming that providers are competent, licensed, and trustworthy. In 2025, credentialing involves collecting and validating an extensive set of documents, including:
-
- State medical licenses, DEA, and Controlled Dangerous Substances (CDS) registrations.
- Board certifications and specialty fellowship records.
- Educational diplomas from accredited institutions.
- Proof of malpractice insurance with adequate coverage.
- National Provider Identifier (NPI) number via the NPPES registry.
- Detailed Curriculum Vitae (CV) outlining work history, affiliations, and publications.
- Peer references (2-3) from colleagues or supervisors.
- Hospital affiliations and privileging documents.
The process relies on Primary Source Verification (PSV), where credentials are confirmed directly with issuing entities, such as medical schools, state boards, or the American Board of Medical Specialties (ABMS). Platforms like CAQH ProView, used by over 1,000 payers, streamline data collection but require meticulous updates. Credentialing typically spans 90-150 days, depending on provider complexity and payer requirements. For example, Medicare mandates CMS-855 forms, while private payers like Aetna and UnitedHealthcare require CAQH profiles.
Understanding Payer Enrollment
Payer enrollment is the process of registering a credentialed provider with insurance companies or government programs (e.g., Medicare, Medicaid) to receive reimbursements for services. It’s the step that integrates providers into payer networks, enabling in-network billing and contracted reimbursement rates. Enrollment involves submitting detailed applications—often overlapping with credentialing documents—and signing payer contracts that outline payment terms.
In 2025, enrollment requires forms like CMS-855I for individual practitioners or CMS-855B for group practices, alongside payer-specific applications for private insurers like Cigna, Blue Cross, or Anthem. The process typically takes 60-120 days, depending on payer efficiency and submission accuracy. Unlike credentialing, which verifies qualifications, enrollment focuses on financial and contractual alignment, ensuring providers are paid promptly for their services.
Enrollment is the gateway to reimbursement. Without it, even a fully credentialed provider cannot bill insurers, resulting in claim denials or reliance on out-of-pocket patient payments. For practices serving Medicare or Medicaid patients, enrollment errors can lead to 20-30% claim rejection rates, significantly impacting cash flow. In 2025, consolidated CMS-855 forms streamline submissions, but expanded requirements for Skilled Nursing Facilities (SNFs) demand precise ownership data.
Key Differences Between Credentialing and Enrollment
While credentialing and enrollment are interconnected, they serve distinct purposes in the medical billing ecosystem. Here’s a comprehensive comparison:
| Aspect | Credentialing | Enrollment |
|---|---|---|
| Purpose | Verifies qualifications (education, licenses, certifications) for competence. | Registers providers with payers for reimbursement and network participation. |
| Focus | Ensures patient safety, compliance, and eligibility to practice. | Establishes financial relationships and billing rights with payers. |
| Key Activities | PSV, CAQH profile updates, hospital privileging, document verification. | Submitting CMS-855 forms, payer applications, and signing contracts. |
| Timeline | 90-150 days, based on verification complexity. | 60-120 days, depending on payer processing times. |
| Stakeholders | Hospitals, medical boards, payers, credentialing committees. | Insurance companies, Medicare/Medicaid, practice administrators. |
| Outcome | Approval to practice and bill as a qualified provider. | Ability to bill payers and receive in-network reimbursements. |
| 2025 Updates | Stricter PSV rules; new CMS requirements for MFTs and MHCs. | Consolidated CMS-855 forms; expanded SNF ownership data requirements. |
Why Both Processes Are Critical for Medical Billing
Credentialing and enrollment are the foundation of a practice’s revenue cycle. Here’s why both are indispensable in 2025:
-
- Revenue Protection: Credentialing ensures eligibility to bill, while enrollment secures payment. Delays in either can lead to $7,000-$10,000 in weekly losses per provider, with unbilled services accumulating rapidly. A 2024 survey reported that 65% of practices face delays, costing millions annually.
- Compliance with Regulations: CMS and private payers conduct audits to verify credentials and enrollment status. Non-compliance risks fines, claim denials, or network exclusion. For example, Medicare’s 2024 rule requiring hospice physicians to be enrolled or opted-out continues to enforce strict oversight in 2025.
- Enhanced Patient Access: In-network providers attract more patients due to lower out-of-pocket costs. Credentialing builds trust by ensuring qualified care, while enrollment makes that care affordable through insurance coverage. Practices with in-network providers see 20-30% higher patient volumes.
- Reduced Claim Denials: Accurate credentialing and enrollment minimize denials, which account for 10-15% of practice revenue losses annually. Skyshine’s integrated approach achieves a 98% first-pass claim approval rate, saving practices thousands.
- Adaptation to 2025 Trends: New CMS regulations, CAQH digital enhancements, and payer-specific requirements (e.g., Cigna’s updated enrollment forms) demand proactive management. Outsourcing to Skyshine ensures compliance with these changes, reducing administrative burdens..
The Credentialing Process: A Step-by-Step Breakdown
To understand how credentialing sets the stage for enrollment, let’s outline its nine key steps, incorporating 2025 standards:
-
- Document Collection (1-3 weeks):
- Gather licenses, certifications, diplomas, malpractice insurance, NPI, CV, and references.
- Update CAQH ProView profiles, mandatory for most payers.
- Educational Verification (2-4 weeks):
- Verify degrees via PSV with medical schools or the National Student Clearinghouse.
- For international graduates, confirm Educational Commission for Foreign Medical Graduates (ECFMG) certification.
- Training Verification (2-4 weeks):
- Confirm residency/fellowship details via program directors or AMA’s FREIDA database.
- Verify board eligibility through ABMS.
- Licensing Check (1-2 weeks):
- Verify state licenses, DEA, and CDS registrations via FSMB or NPDB.
- Work History Review (3-5 weeks):
- Validate 5-7 years of employment, explaining gaps over 6 months with affidavits.
- Confirm hospital affiliations and privileges.
- Malpractice History (2-3 weeks):
- Query NPDB for claims, settlements, or judgments; disclose all incidents.
- Ensure adequate coverage for the provider’s specialty.
- References and Background Checks (1-2 weeks):
- Secure 2-3 peer references from colleagues familiar with the provider’s work.
- Run FCRA-compliant criminal background checks and check OIG exclusion lists.
- Committee/Payer Review (4-8 weeks):
- Submit to hospital credentialing committees or payers via CAQH or direct applications.
- Approval and Maintenance (Ongoing):
- Receive approvals; re-credential every 2-3 years per payer or hospital policy.
- Update CAQH profiles quarterly and report changes (e.g., address, licensure) promptly.
- Document Collection (1-3 weeks):
Skyshine’s Role: Our team handles all steps, leveraging automation and established relationships with verification bodies to achieve approvals in 60-80 days, compared to the industry average of 120 days. Our 98% first-pass approval rate minimizes delays and ensures compliance.
The Enrollment Process: A Step-by-Step Breakdown
Once credentialed, enrollment connects providers to payers for billing. Here’s the five-step process:
-
- Application Preparation (1-2 weeks):
- Complete CMS-855 forms (e.g., CMS-855I for individuals, CMS-855B for groups) and payer-specific applications.
- Include credentialing documents like NPI, licenses, and CAQH profiles.
- Payer Submission (1-2 weeks):
- Submit applications to Medicare, Medicaid, or private payers (e.g., Aetna, Cigna, Blue Cross).
- Contract Negotiation (2-4 weeks):
- Review and sign payer contracts outlining reimbursement rates and terms.
- Verification and Approval (4-6 weeks):
- Payers verify enrollment details, cross-referencing credentialing data.
- Ongoing Maintenance (Ongoing):
- Revalidate enrollment every 3-5 years per CMS rules.
- Report changes (e.g., practice address, ownership) within 30 days to avoid penalties.
- Application Preparation (1-2 weeks):
Skyshine’s Expertise: We submit to multiple payers simultaneously, using tailored templates to meet unique requirements, securing approvals in as little as 4 weeks. Our team also monitors revalidation deadlines, ensuring zero disruptions.
Optimizing Credentialing and Enrollment in 2025
To streamline both processes and maximize billing efficiency:
-
- Start Early: Begin 4-6 months before a provider’s start date to account for delays. Early action can save $50,000-$100,000 in potential revenue per provider.
- Leverage Technology: Use platforms like Symplr, Modio Health, or CAQH ProView for document management and tracking. Skyshine’s proprietary software integrates these platforms, reducing administrative time by 50%.
- Outsource to Experts: Partner with Skyshine to offload administrative burdens, achieving 30-50% faster approvals and a 98% approval rate.
- Monitor Updates: Stay informed on CMS, CAQH, and payer changes via newsletters or consultants. Skyshine’s team provides real-time compliance updates.
- Integrate with RCM: Align credentialing and enrollment with billing, coding, and denial management to reduce denials and boost cash flow. Skyshine’s end-to-end RCM approach saves practices 10-15% in annual losses.
2025 Trends: Digital platforms like CAQH ProView and PECOS are streamlining submissions, but stricter PSV rules and new provider requirements demand vigilance. For example, CMS’s 2024 consolidation of CMS-855 forms simplifies submissions but requires precise ownership data for SNFs. Telehealth providers face additional enrollment scrutiny, with payers like Cigna requiring specialized compliance forms. Skyshine’s expertise ensures practices stay ahead of these trends.
Conclusion: The Power of Credentialing and Enrollment
In 2025, provider credentialing and payer enrollment are not just administrative tasks—they’re strategic imperatives that drive revenue, compliance, and patient access. While distinct, these processes are interdependent, forming the foundation of a robust revenue cycle. Credentialing verifies a provider’s qualifications, ensuring trust and eligibility, while enrollment connects them to payers, enabling reimbursements. Together, they reduce denials, enhance cash flow, and support practice growth.
By understanding their differences, addressing challenges, and leveraging expert support, practices can minimize delays and thrive in a competitive landscape. Skyshine Health Solutions is your trusted partner in this journey. Our proven expertise ensures faster approvals, higher accuracy, and seamless billing integration. Ready to optimize your practice’s financial health? Contact Skyshine today for a free credentialing and enrollment audit and discover how we can save you time and money.

Check our blog on Why Credentialing Verification Matters in medical billing 2025
Call to Action: Visit Skyshine Health Solutions to schedule your free consultation and streamline your credentialing and enrollment processes for 2025 success.